|
| diasource-diagnostics.com |
The common tests are:
1.Serological testing
2.Urea breath test
3.Biopsy based urease
4.Histology
5.Microbial culture
1/ This detects antibody (IgG) response to H.pylori antigens. This confirms exposure at some point but will not discriminate between current or previous exposure. Therefore it can not be used to follow up eradication therapy.
2/This relies on bacterial urease activity in the stomach which is only found if H.pylori is present. Radiolabelled urea is ingested and is then broken down by the urease. Radiolabelled carbon dioxide is released into the blood and subsequently exhaled. This test can be used to asses active infection but has time and cost implications in primary care.
3/This uses the same principle as the urea breath test. Tissue biopsy containing urease is placed in a urea solution. Ammonia is released which raises the pH of the solution which is detected by an indicator. This is the basis of the CLO (campylobacter like organism) test. A major diadvantage of this test is that it involves an invasive endoscopic procedure.
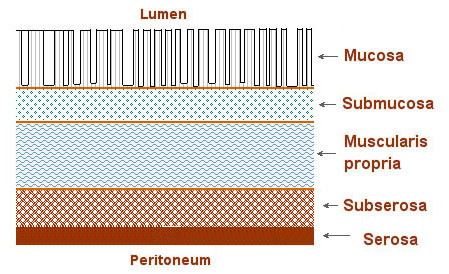
4/This requires visualisation of H.pylori adherent to the gastric mucosa. The bacteria can be directly viewed using HandE staining. Alternatively, specific stains or immunological techniques can be used. Disadvantage: the test is invasive. Advantage: culture and sensitivity to the most commonly used agents (clarithromycin and metronidazole) can be performed.
5/Faecal antigen testing requires the detection of H.pylori antigens shed from live bacteria into the gut lumen.